SCIENCE
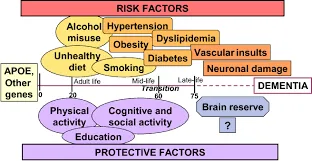
Prevention of Cognitive Decline. Dale E Bredesen1*, et al.
Please click on the link above to read the article.
Inside the FINGER Study : Hard Evidence Shows How Diet, Exercise and Mind Games Might Make or Break a Dementia Diagnosis. Miia Kivipelto.
Please click on the link above to read the article.
Detailes about FINGER intervention.
DIAGNOSTICS
Initial LABS
• ApoE4 status; whole exome, exome chip, or genome.
• Homocysteine
• Hemoglobin A1c, fasting insulin
• Lipid Panel :
- Total Cholesterol, HDL, Triglycerides, LDL-Cholesterol (calculated), Cholesterol/HDL Ratio (calculated), Non-HDL Cholesterol (calculated)
• Complete Metabolic Panel :
- Albumin, A/G Ratio, Alkaline Phosphatase, ALT, AST, BUN/Creatinine Ratio, Calcium, Carbon Dioxide, Chloride, Creatinine with GFR Estimated, Globulin, Glucose, Potassium, Sodium, Total Bilirubin, Total Protein, Urea Nitrogen , Hs-CRP (high sensitivity C-reactive protein)
• Hormone status:
- estradiol, DHEA-S, total testosterone, free T3, reverse T3, free T4, TSH, progesterone, cortisol
• Vitamin D
• Vitamin B12, folate
• Vitamin E (Vitamin A, E, b-carotenold Panel) • Heavy Metals Panel: (Hg, Pb, As)
• Zinc
• Copper
• RBC Mg
• MMP9
ReCode INTERVENTION


KetoFLEX 12/3 Nutrition Summary
KetoFLEX 12/3 is a diet (that becomes a lifestyle) to optimize cognition.
- Keto refers to ketosis, the natural process by which your body breaks down its own fat to use as fuel.
- FLEX refers to metabolic flexibility, the ability to use either glucose or fat as a fuel source. FLEX also refers to a flexetarian diet, in which meat is optional.
- 12/3 refers to the minimum amount of time each day that you should spend fasting; for at least 12 hours with at 3 hours before bed.
How does KetoFLEX 12/3 help my brain?

- The three components of the KetoFLEX 12/3 lifestyle are: diet, fasting, and exercise on a foundation of quality sleep.
- When combined, they heal metabolism and provide clean sustainable fuel for your brain.
- You can test your blood glucose and ketones to track your progress.
How do I get started?
- Eliminate all sugar, simple carbohydrates, conventional dairy and grains (with some exceptions in Chapter Five ).




What am I supposed to eat on KetoFLEX 12/3?

- Fast for at least three hours before bed for a minimum of twelve hours.
- ApoE4 carriers may want to try to extend their fast to 16+ hours.
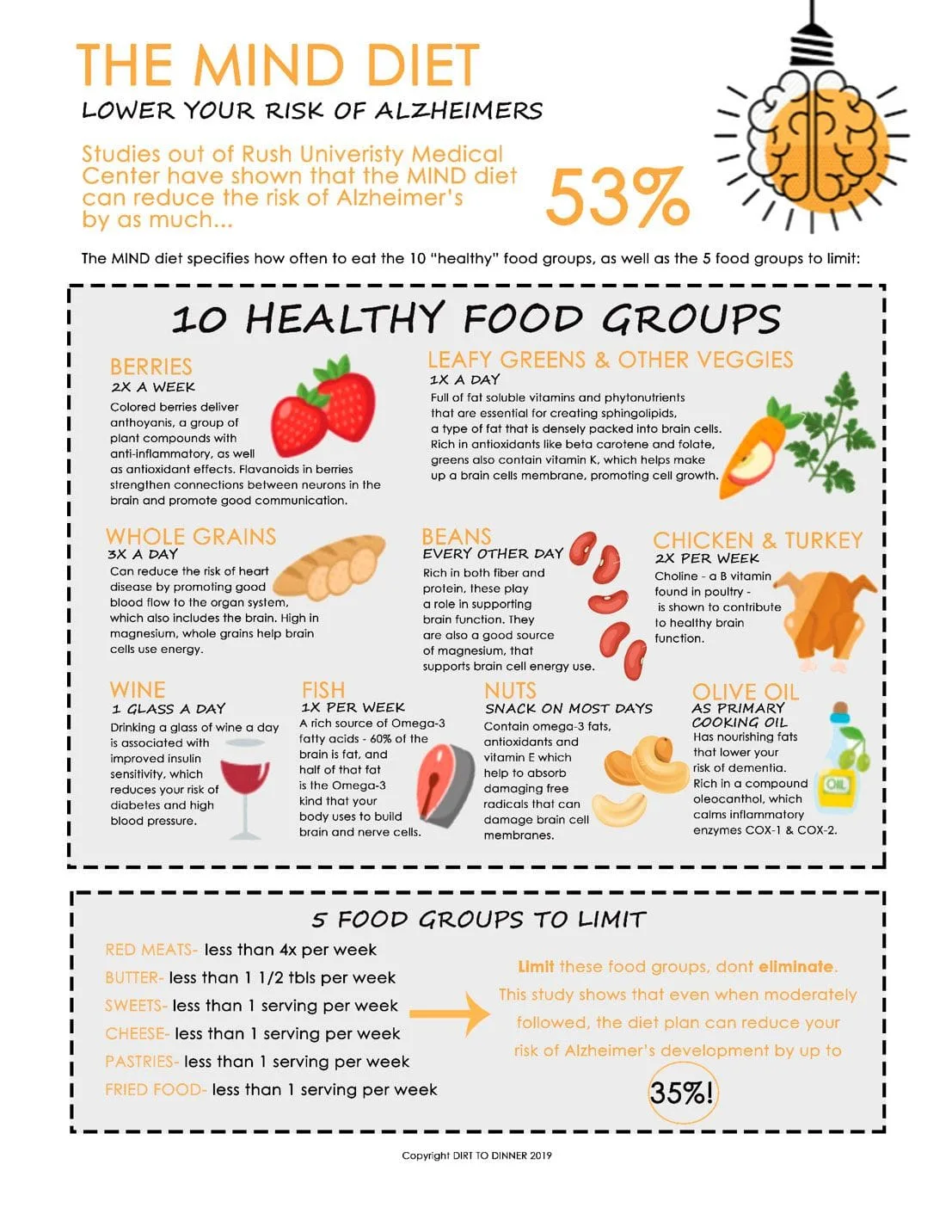
- Eat at LEAST 6-9 cups of deeply pigmented, organic, seasonal, local non-starchy vegetables per day, increasing the amount as tolerated.
- Challenge yourself to bring home one novel vegetable (or new variety of a familiar vegetable) each time you shop to expand your repertoire.
- Include leafy greens, especially those that produce nitric oxide.
- Include cruciferous vegetables, paying careful attention to preparation to maximize health benefits.
- Include fresh herbs, spices, and teas.
- Increase healthy fat (with increased plant intake) to heal insulin resistance while creating ketones to fuel your brain.
- Prioritize high polyphenol EVOO, avocado, and nuts.
- Remember not to combine high glycemic and inflammatory foods with dietary fat.
- Be aware that as you heal, your need for dietary fat may decrease over time.
BFP Level Three: Upgrade Your Gut
- If you have any chronic GI issues: work to address root causes, incorporate strategies to optimize digestion, and consider a three week elimination diet (including FODMAPs if necessary) to identify hidden food sensitivities.
- Slowly incorporate foods with prebiotic fiber into each meal.
- If resistant starch is appropriate for you, look for opportunities to add small amounts into your diet using healthy fats to reduce the glycemic effect if necessary.
- Once insulin sensitivity, gut health have been remediated, a long term goal is the incorporation of more resistant starches.
- Experiment with adding a variety of probiotic foods into your diet.
BFP Level Four: Choosing Wisely
- Healthy people should limit protein consumption to 0.8-1.0 gram per kilogram of lean body mass per day with some exceptions outlined in The KetoFLEX 12/3 Nutrition Guidelines Chapter Six .
- Be aware that protein goals may be reduced as healing progresses to enhance autophagy.
- All plants contain some protein. There is no need to limit your protein from whole plants.
- Prioritize wild-caught seafood and pastured eggs.
- Eat heirloom fruit seasonally. Depending upon what part of the world you live in, there may be many other options available. Always balance nutritive value against glycemic concerns.
- Enjoy small portions (1/2 cup or less) of wild berries year round.
- Unripened tropical fruit (green plantains, bananas, mangoes, papayas, and kiwi) may be eaten in small amounts as resistant starch and for their natural digestive enzymes.
- Lemons and limes are great sources of vitamin C and can be enjoyed liberally.
- If necessary, use limited amounts of approved sweeteners.
- To derive the health benefits of flavanols, enjoy small amounts of high cacao chocolate, low in sugar, cadmium and lead.
- Because of toxicity concerns, limit cacao nibs and avoid cocoa and cacao powder.
- Consider a flavanol supplement.
- Avoid all conventional dairy.
- You may have small amounts of A2 dairy if tolerated and desired.
- Alcohol is a neurotoxin and best avoided by anyone at risk of or suffering with cognitive decline.
- If you decide to occasionally indulge, consider small amounts of organic sugar-free, low alcohol red wine.
For those interested in the full details of the KetoFLEX 12/3 diet, please read through our complete Nutrition Guidelines .
© 2019 AHNP, LLC. Certain digital content herein is derived or adapted from portions of publications by Dale E. Bredesen. All rights reserved. No part of this site or the content herein may be reproduced or reprinted without prior written permission from AHNP, LLC.
Nutrition Guidelines – Ketoflex 12/3
Nutrition is an important contributor to a lifestyle that optimizes cognition and well-being. What and when you eat, and don’t eat, how well you sleep, move and handle stress, experience joy, are all intricately connected and function together with this program. There are patients who have implemented only the basics of these guidelines and seen reversals of their cognitive decline, while there are others who have needed strict adherence to induce and sustain cognitive improvement.
Ketoflex 12/3 is based on a “ketogenic” lifestyle. That is, creating ketosis, a fat-burning state that produces ketones. Ketones are the preferred fuel, over glucose, for the brain as they are more efficient (absorbed faster) and clean (produce fewer free radicals or oxidative damage). Most critical is the observation that the brain demonstrates a decrease in glucose utilization in the Alzheimer’s disease regions for decades before cognitive decline is noted. This deficit is often caused by insulin resistance, which also leads to a difficulty shifting from one fuel source to another. In the midst of this deficit, the brain can still utilize ketones to compensate for this shortfall in fuel. Our goal of “metabolic flexibility” allows for a seamless transition from one fuel source to the other.
Ketosis is safe and natural. Babies are naturally in ketosis much of the time (human breast milk is high in medium chain triglycerides (MCT), which support ketosis) as are metabolically flexible adults during sleep, fasting, and exercise. Ketones have been used as fuel throughout much of human history. Only in modern times have people eaten three highly refined meals a day, plus snacks, while becoming increasingly sedentary. In many non-Westernized parts of the world, people still live a ketogenic lifestyle. They are active throughout the day, often performing physically demanding labor. They eat much less often, partaking of traditionally prepared whole food with periods of fasting both daily, and intermittently, imposed with seasonal food supplies.
Ketones are produced by fasting 12/3 (see below), minimizing refined carbohydrates, proteins, increasing good fats and exercising. The program is also “flexitarian” in that, although it is a primarily plant-based diet, it does allow limited, clean sources of animal products. The pace at which these changes are adopted depends on your readiness and willingness. They can be implemented slowly over weeks, months, or all at once. Those making the transition quickly have the opportunity to promote healing more rapidly, but must be aware of the possible, usually mild and transitory, side effects that can result. Dehydration (and the subsequent mineral loss) is behind most of the transitional side effects, often dubbed the “keto-flu.” It’s especially important while transitioning, and for the entirety of your adoption of these guidelines, to stay hydrated and to supplement with sea salt* to replenish lost minerals. Here’s a helpful resource with a comprehensive list of possible side effects and tips on how to avoid them.
*When choosing a non-iodized salt, be sure to get enough iodine through your diet from sources like fish and sea vegetables.
A. FASTING
Fasting is incorporated into the Ketoflex 12/3 program daily as it allows for optimizing many critical metabolic functions by controlling when you eat. Fasting helps induce ketogenesis, the fat-burning state that produces ketones. Fasting allows autophagy (“self-eating”) to occur, which is a process that removes damaged proteins and thereby contributes to detoxification. Detoxification is critical to all of us in our modern world with the cumulative burden of toxicity, but especially urgent to those suffering from neurotoxicity.
1) Fast for at least 12 hours between the end of dinner and the beginning of breakfast. ApoE4 carriers may want to work towards extending the fast to 16 hours. Coffee or tea drinkers may freely enjoy a cup or two of organic black coffee or tea (with a limited amount of stevia, if desired) while still essentially fasting. Both coffee and tea are high in antioxidants and associated with longevity. Caffeine drinkers experience increased cognitive clarity, energy, and mood. It is best to break the fast, when hungry, with water (not cold) with some lemon, ginger, green tea and/or other detoxifying drink.
2) Fast for at least 3 hours prior to going to bed. As the day winds down, the body needs less food for energy and should be entering a fat-burning state. This fat-burning state will facilitate your body’s detoxification and repair. Sleep provides an opportunity to add hours to a total fasting time and helps to mimic our ancestral circadian (daily) rhythms by fasting with the setting of the sun and eating with the height of the sun.
3) Note that fasting is especially difficult to initiate, particularly for those with insulin resistance. Insulin resistance creates a state in which your body is less able to use the sugar you are providing it, and this can create carbohydrate craving. There are several methods that have been shown to help with hunger, carbohydrate cravings, and ultimately to increase insulin sensitivity. MCT, such as coconut or MCT oil, are saturated oils that are rapidly absorbed and especially useful for overcoming glycotoxicity (sugar toxicity and insulin resistance). It is best to increase the amount from one teaspoon or less to one tablespoon gradually (once to three times per day) to avoid side effects. Another way to mitigate hunger is with healthy fats, such as a handful of nuts or seeds, avocado slices, or non-starchy vegetables. When you become insulin sensitive and familiar with the sensation of being in ketosis, you do not experience the urgency of hunger. Exercise can be helpful in increasing insulin sensitivity, making fasting easier over time.
For Information about Fasting Mimicking Diet click here
To order Prolong click here
B. MINIMIZE SIMPLE CARBOHYDRATES
Simple carbohydrates, such as sugar and processed foods, stimulate the production of insulin and can create insulin resistance. Insulin resistance impairs the brain’s ability to use glucose as an energy source, and the associated high glucose leads to inflammation. Increasing the use of fats as a source of fuel for the brain, which the brain uses more efficiently, while decreasing insulin resistance, is a critical component of the nutrition guidelines. Decreasing insulin resistance is achieved by avoiding simple carbohydrates, sugar, and processed foods while increasing nutrient and fiber-rich foods, such as those found in plants.
It is key to minimize simple carbohydrates (sugar, candy, cookies, muffins, cakes, all bread, pasta, white potatoes, grains, soft drinks—both regular and diet (artificial sweeteners disrupt the gut microbiome)—fruit juices, alcohol, processed foods, and anything with high fructose corn syrup). It’s OK to eat sweet potatoes and other colored potatoes in limited amounts. As you limit your intake of simple carbohydrates, you will lose your desire for sweet-tasting food. Organic stevia, in a relatively pure form, may be used as a sweetener in small amounts. (SweetLeaf is one recommended brand.)
Carbohydrates can be categorized as simple (sugars or carbohydrates that break down easily into sugars), complex (starch or carbohydrates that do not break down as easily) and fibers (plant material that does not break down in the human gut). A “resistant starch” is a complex starch that behaves more like a fiber. Resistant starches resist digestion (by humans, but not by some bacteria in your colon), and thus do not contribute as significantly to your blood glucose. Many plants, roots and tubers contain various ratios of these resistant starches and fibers. Some potatoes, other root vegetables, rice, and legumes can be converted from a complex into a resistant starch by cooking, then cooling. (Reheating is debated; some claim that the resistance of the starch is compromised, especially if heated to over 130 degrees.)
C. EAT WHOLE FOOD, MOSTLY PLANT-BASED
1) VEGETABLES: The majority of your diet should be comprised of non-starchy vegetables with some limited starchy vegetables. The chart below outlines some of your key options to guide your choices. Vegetables in green should be enjoyed freely. Vegetables in yellow and red should be limited and monitored for their potential to negatively affect glycemic markers.
Choose colorful, deeply pigmented, seasonal, local, non-GMO and organic to the extent possible. The Environmental Working Group’s Dirty Dozen , Clean Fifteen list can help to guide organic selection priority.
| Vegetables | Cruciferous Vegetables | Herbs/Spices | Resistant Starches |
|---|---|---|---|
| Artichokes | Arugula | Basil | Beans/Lentils** |
| Asparagus | Bok choy | Bay leaves | Cassava |
| Beets* | Broccoli | Chives | Celery root |
| Beet greens | Broccolini | Cilantro | Green banana |
| Carrots* | Brussels sprouts | Cinnamon | Green mango |
| Celery | Cabbage | Coriander | Green papaya |
| Cucumber | Cauliflower | Cumin | Green plantain |
| Chickory | Collard greens | Dill seed/weed | Jicama |
| Eggplant | Dandelion greens | Ginger | Millet*** |
| Endive | Horseradish | Lavender | Parsnip |
| Escarole | Kale | Marjoram | Potato starch |
| Fennel | Kohlrabi | Mint | Rice*** |
| Garlic | Maca | Oregano | Rutabaga |
| Green Beans | Mustard greens | Parsley | Sorghum*** |
| Hearts of Palm | Raddichio | Rosemary | Sweet potato |
| Jicama | Radish | Saffron | Taro root |
| Leeks | Rapini | Sage | Turnip |
| Lettuces | Swiss chard | Tarragon | Yam |
| Mushrooms | Wasabi | Thyme | Yucca Root |
| Okra | Watercress | Turmeric | |
| Onions | |||
| Peas | |||
| Peppers | |||
| Purslane | |||
| Scallions | |||
| Sea vegetables | |||
| Snap peas | |||
| Snow peas | |||
| Spinach Squash* | |||
| Zucchini |
*Consuming raw or lightly cooked reduces glycemic impact.
**Pressure-cook to reduce lectins. Lectins are “sticky proteins” that cause holes in our gut leading to “leaky gut”.
***These are allowable grains due to their low lectin content and beneficial resistant starch.
Plants are the cornerstone of this program for a multitude of reasons. When plants are grown in healthy soil, a synergy of thousands of compounds occurs that creates remarkable phytonutrients, some of which we have yet to understand. These “whole foods” cannot be replaced with supplements. In addition, we now understand that the brain and gut are intricately, and bi-directionally, connected. The health of the brain begins with the health of the gut, and gut health begins by promoting a beneficial microbiome. Beneficial bacteria, given an opportunity to feast on these healthy plants, thrive and heal the gut, among many beneficial effects.
Leafy green vegetables* are found in the vegetable, cruciferous, and herb/spice columns. They are at the top of the nutrient density chart for optimal health, and contribute to brain health with many of these nutrients: Vitamins K, C, A and carotenoids such as lutein, beta-carotene and zeaxanthin, which have all shown evidence for contributing to cognition and preventing its decline. Vitamin B9 (folate, which comes from the term “foliage”), when combined with B12 and B6, reduces homocysteine, a metabolite that is measured on the protocol. Evidence has revealed that an elevated homocysteine corresponds with progressive atrophy of the hippocampus, a critical structure for memory.
Colored vegetables impart their value as antioxidants based on their pigments: carotenoids are yellow and orange, flavonoids are red, blue, purple, black and cream, and chlorophyll are green. The deeper and more widespread the pigment throughout the vegetable (or fruit), the more nutrients are typically present.
*A warning to those on Coumadin (Warfarin): Your physician should approve and monitor any change in intake of vitamin K-rich foods, like leafy green and other vegetables (and some fruits). Coumadin works as a blood thinner by interfering with vitamin K, and sudden increases may change the effectiveness of the drug!
Cruciferous vegetables* are some of the most powerful and nutrient dense vegetables. It is the sulfur component of cruciferous vegetables that gives some bitter taste, but is responsible for many of the health merits. Sulfur is required for the synthesis of glutathione (the “master antioxidant” for detoxification in the liver) and the production of several amino acids that provide the structural component of many tissues and hormones, including insulin. The alliums (onions, shallots, garlic, leeks) and the brassicas (cabbage, broccoli, cauliflower, Brussels sprouts, bok choy) aid in detoxification, protect from oxidative damage, and improve glucose metabolism. When cruciferous vegetables are chopped, juiced and chewed, their unique sulfur compounds areconverted and released. They are best consumed blanched, lightly steamed, sautéed at medium heat to preserve crunch, or added to soups and stews.
*Raw cruciferous vegetables are known to inhibit iodine uptake. The thyroid gland preferentially binds iodine for its function. As iodine deficiency is thought to play a role in thyroid disease, these vegetables should be at least minimally cooked.
Mushrooms, often considered vegetables, are actually important and unique edible fungi that have been prized throughout the ages and cultures for their medicinal and flavor qualities. Not only do they contain sulfur, but they are also rich in Vitamin B and beta-D-glucan. Beta-D-glucan is important to the innate immune system (the ancient part of our immune systems, which functions as a first responder), which is thought to play a role in the reversal of cognitive decline. Immune-enhancing effects are present in nearly all mushrooms including white button, cremini, portobello, shitake, reishi, chanterelle, oyster and many others. Mushrooms are heat-stable and therefore, still nutritious while adding flavor when cooked with garlic, onions and vegetables.
Herbs and spices, which contain antiviral and antimicrobial properties, are an integral part of cooking with whole foods. Most contain more disease-fighting antioxidants than fruits and vegetables. It’s best to source fresh and organic herbs and spices as they have the most nutritional value.
Fiber and resistant starches are naturally present in a diet high in vegetables. Fiber and resistant starch are the components of the plants that are digested by the beneficial bacteria. Their by-products provide us with SCFA (short-chain fatty acids) and ketones that are excellent fuels, products that contribute to the integrity of the gut lining, the regulation of the immune system, and thus to brain health. They help us feel full and regulate bowel function.
______
Everyone, but especially those healing from insulin resistance or working to switch from a carbohydrate-based diet to a fat-based diet, may need to proceed cautiously with resistant starches, legumes, and quinoa, since these may spike glucose levels. You may not be able to include any of these at the onset, or move toward a limited amount as you achieve insulin sensitivity. It may be necessary to check for glucose levels to assess how you respond to a given amount of these foods, such as not to negate your earned gains.
______
Note: if you are ramping up your intake of vegetables, your microbiome will be changing; therefore, do so gradually as your system may need to adjust its production of enzymes to handle the change. Also, see under Gut Health for concerns about food allergies or intolerances.
2) FRUITS:
The best fruits are wild berries, lemons, limes, tomatoes, olives and avocados.As whole fruits (not juices) are high in nutrient density and fiber, they can be used as a dessert at the end of a meal containing dietary fat. Organic, wild berries, in reasonable portions,* should be prioritized as their polyphenolic compounds have been shown to have a therapeutic role in both preventing and remediating cognitive decline. Ancestrally, fruits were consumed at the end of summer to fatten for the winter. Avoid or limit tropical fruits (except for green bananas, mangoes, papaya and plantains in limited amounts as resistant starch) because of their increased glycemic indices. Avocados are an extraordinary standout in that they are high in nutrients, fiber, and beneficial fats. They will not induce glucose spikes, and can help you achieve a ketotic state. They can easily be added to every meal and needn’t be organic due to their thicker skin.
*Due to the potential for glycemic spikes.
A note about alcohol. Epidemiological studies suggest that a glass of wine per day may be both cardio and neuro-protective. However, in terms of cognitive health, existing evidence is insufficient to suggest that those who currently abstain should begin to drink alcohol. It is important to emphasize that all alcohol is a neurotoxin. Focused research has shown that ApoE4 carriers do poorly with any amount of alcohol. If you choose to indulge occasionally, limit yourself to a few ounces of dry red wine with or following a meal to blunt the glycemic effect. For anyone with a history of alcohol abuse, it is best to abstain completely.
3) NUTS and SEEDS:
Nuts and seeds are powerhouses of nutrition. They have been found to be both cardio and neuro-protective and contain an excellent fat, protein, vitamin, mineral and fiber content. Nuts and seeds should be fresh, organic, raw, ( soaked and sprouted when possible, as these methods will reduce lectins, phytates and enzyme inhibitors, all of which will impair digestion and nutrient absorption). It is best to dehydrate or roast at low temperatures, 170-220 degrees F (77-104 degrees C), with the type of nut or seed dictating the timing. When oven roasting, periodically turn the nuts and seeds to ensure even cooking. You can experiment with tossing your raw nuts and seeds with various spices, such as paprika, cumin, curry and sea salt prior to roasting to create a healthful and flavorful artisanal snack or meal accompaniment.
When you can’t prepare your own nuts and seeds, buying dry roasted (with no added oils) is the next best option. All nuts and seeds have varying ratios of the different types of fats: monounsaturated fatty acids (MUFA), polyunsaturated fatty acids (PUFA), and saturated fat acids (SFA). PUFAs are particularly susceptible to oxidation and rancidity when exposed to higher commercial roasting temperatures, leading, in turn, to inflammation. Nuts that are roasted with added, unhealthy oils (for example, seed oils; see below) are not recommended. Storing larger quantities of nuts and seeds in the freezer and smaller quantities in the refrigerator helps preserve freshness.
Walnuts, macadamia nuts, pistachios, pecans, almonds, hazelnuts, brazil nuts, pine nuts, cacao (used as nibs or powder) and seeds of pumpkin, sunflower, sesame, black sesame, flax, hemp, quinoa and chia are all excellent options.
- Walnuts have been especially associated with brain health because of their high omega-3 fatty acid content, but should be consumed raw since PUFAs oxidize easily.
- Flax seeds, also high in omega-3 fatty acids, must be eaten raw and either freshly ground or soaked overnight.
- Macadamias have the highest MUFA content and a low carbohydrate, protein, and lectin (plant toxin) content.
- Pecans also are excellent for their high healthy fat to carbohydrate and protein ratio.
- Cacao nuts (as cacao nibs, powder or butter), especially raw, are another star in brain health for their healthy fat, nutrient density, metabolic enhancing effect, and flavonols. They have nearly 4x the antioxidant impact of dark chocolate. Dark chocolate (86% or higher) is also excellent.
Try not to consume more than a couple of handfuls or ounces of nuts and a few tablespoons of seeds, unless weight maintenance or gain is desired. It is important to make sure that any nut or seed does not have a rancid or moldy smell. Avoid peanuts (especially peanut butter), which are legumes, and are associated with mold contamination and the resulting inflammation.
4) LEGUMES:
Legumes are helpful for vegetarians and vegans for their protein, mineral and fiber content. Furthermore, since their fiber content is higher than most grains, they do not contribute as much to insulin resistance. Legumes, however, can be problematic because they contain lectins, phytates, and enzyme inhibitors, which contribute to inflammation and impair digestion/nutrient absorption. The lectins and phytates can be mitigated by soaking dry beans overnight (including a four-inch strip of kombu, a seaweed that helps to make the beans more digestible, less gas-producing, and increases the absorption of the nutrients). Following the overnight soaking, the beans can be boiled, according to instructions for whichever type of beans you have soaked. Pressure cooking can also be used.
5) FATS: There are four main types of fat:
- Monounsaturated fatty acids (MUFA): e.g. avocados, olives, nuts and seeds
- Polyunsaturated fatty acids (PUFA; include omega-3 and omega-6): e.g. nuts, seeds, seed oils, algae and fish
- Saturated fatty acids (SFA): e.g. animal fats and coconuts
- Trans fats: synthetic hydrogenated fats, e.g. “partially hydrogenated oils” as seen on the ingredient list of food packages
Trans fats are the only clear-cut demons here. The other fats, under the right circumstances (depending on processing methods, heat extraction, sourcing, presence of low-carbohydrate, high-fiber intake and a good omega 6:3 ratio), can be a substantial, even majority portion (calorically) of your diet leading to a healthy cardiovascular profile. It may be helpful to adjust to your fat intake by increasing slowly. The use of digestive enzymes may also be helpful.
Examples of good fats:
- Extra Virgin Olive Oil (high polyphenol, with a known harvest date, cold pressed, stored in a dark bottle)
- Avocados and avocado oil
- Coconut and coconut oil* (preferably organic, cold-pressed, unrefined, without chemical processing)
- MCT Oil*
- Red Palm Oil* (virgin, unrefined, certified sustainable)
- Walnut oil
- Macadamia oil
- Nuts
- Seeds
- Sesame oil
- Perilla oil
- Algae oil
- Cod liver oil
- Butter* (grass-fed, clarified, goat, sheep, or A2 cows)
- Ghee*
- Cacao Butter*
- Egg yolk* (pastured, organic)
*SFA has been shown to elevate LDL particle number (LDL-P) and ApoB, especially in ApoE4 carriers. This leads to a paradox: on the one hand, MCT oil and coconut oil (both saturated fats) can help to induce ketosis, which is supportive of cognitive function; on the other hand, the resulting increase in LDL-P may be associated with cardiovascular disease. Therefore, one resolution to this paradox is to use MCT oil and coconut oil transiently, to produce ketosis and improve cognition. When this has been achieved, a switch to primarily MUFAs and PUFAs (EVOO, avocados, olives, nuts and seeds) to achieve a continuation of mild ketosis while tracking LDL-P, ApoB, or sdLDL and oxidized LDL may offer continued neuroprotection while concurrently protecting the cardiovascular system. It may be noted that healthy fats in the context of the ketogenic lifestyle often results in a lowering of triglycerides, a rise in functional “good” HDL, and a shift in LDL to the larger, more fluffy particle type, all of which are known to be cardioprotective.
When making dietary fat choices, consider prioritizing fresh, high polyphenol, extra virgin olive oil* (EVOO). Polyphenols are phytochemicals, compounds found abundantly in natural plant food sources, that have antioxidant properties that protect the cells from free radical damage. Polyphenols are believed to be a key component of EVOO that contributes to it’s cardio and neuroprotective properties. Growing evidence suggests that EVOO may play a therapeutic role for reducing neuroinflammation and upregulating autophagy to help with beta-amyloid clearance. Always buy EVOO with a known harvest date; either printed on the bottle or guaranteed by the distributor. EVOO should only be used as a finishing oil (served at room temperature). It is wonderful to pair with low glycemic vinegars or citrus to make a salad dressing. It can also be seasoned with fresh herbs and spices to create a topping or dip for your vegetables. Although it is not recommended to cook with EVOO, if you choose to do so, keep temperatures low to prevent oxidation.
* Amphora Nueva is a good source. They regularly import the highest polyphenol count and freshest harvest from all over the world. Call directly (925) 310-4681 to ensure that you’re getting both.
- Avoid all seed, grain, and bean oils (polyunsaturated, omega-6, heat-extracted and GMO refined oils) such as soy, corn, canola, peanut, sunflower, safflower, cottonseed, and palm kernel.
- For cooking oils, choose oils with high “smoking” points, that do not produce smoke at higher temperatures. Good choices are avocado oil, coconut oil, butter, ghee, or animal fat.
- Avoid all trans fats processed foods such as crackers, cookies, cakes, chips, microwave popcorn, frozen dinners, pizza, creamers, margarine, cool whip, and all fast food. (Food manufacturers can claim 0 trans fats on the label even though they may include up to 0.5 grams/serving.)
6) PROTEIN:
Use animal protein as a condiment, not a main course. We need protein for essential body functions, but it’s important to realize that the average American eats too much. It’s important to limit your protein consumption to 0.8 to 1 gram of protein per kilogram of lean body weight per day*. The actual protein needs for each person are highly individualized. Those with underlying illness (especially suboptimal gastrointestinal (GI) function) may temporarily need to stay near the maximum recommended level while they heal. As health is optimized, protein requirements will be reduced. To prevent muscle loss while reducing protein, it’s vital to incorporate strength training into your lifestyle. Look for opportunities to add weight-bearing movement into your day. Much of your protein needs can come from plants. Two cups of spinach nearly equals the equivalent of 2 pastured eggs, but plant protein is often incomplete and less bio-available. Vegetarians and vegans can achieve adequate protein in vegetables, nuts, seeds, tempeh, and beans, but should consider potential deficiencies in omega-3, vitamin B-12, vitamin D and choline.
*Determine your lean body weight using this calculator . Choose an average of the three results, then use this tool to convert to kilograms. Use CRON-O-meter to determine the amount of protein in a given food.
There are justified debates over the issues of the consumption of animal protein. However, for the purpose of reversal of cognitive decline, the use of omega-3 fatty acid, especially DHA, is critical. DHA is one of the most important fats for the brain since synapses (neuronal connections) need DHA for their structure. In other words, DHA helps promote new brain cell growth and protects existing brain cells. An excellent source of DHA is cold-water fatty fish. Fish should be wild-caught, high omega-3, and low in mercury. It’s helpful to remember the “SMASH” (salmon, mackerel*, anchovies, sardines**, and herring) acronym when choosing fish. Salmon has high omega-3 and low contamination. Best sources are wild-caught Alaskan and sockeye. High-mercury fish are typically those with long lives and large mouths, such as tuna, swordfish, and shark, and should be avoided. In general, fish that are smaller and lower on the food chain are the safest. Carefully source your shellfish, crustaceans, and mollusks. Most are wild-caught, with the exception of shrimp. Avoid farmed shrimp. There are sites such as the Monterey Bay Aquarium Seafood Watch, Marine Stewardship Council, Natural Resources Defense Council, and labels such as Fishwise and Seafood Safe, to guide you in your choices of less toxic and sustainably harvested fish.
*Atka & North Atlantic caught mackerel from the US & Canada are low in mercury. King & Spanish Mackerel should be avoided as they are high in mercury.
**Sardines should be sourced from the Pacific Ocean.
When using animal protein*, it is important to use organic, pastured, high omega-3 sources, which means that the animals have not been subject to CAFOs (concentrated animal feeding operations) with the inherent inflammation/toxicity of antibiotics, growth hormones, stress, feed and living conditions unnatural to those animals. Given that virtually all poultry and livestock are raised in CAFOs, sourcing healthy protein from animals is a challenge. However, for many it is a challenge worth pursuing, especially when it comes to finding eggs from 100% pastured hens. Eggs are one of the best sources for choline, a micronutrient, critical to the brain in that it stimulates the production of acetylcholine, a neurotransmitter responsible for synaptic connections (i.e. memory).
*“American Grassfed” is a label that denotes pasture-raised. ButcherBox is one resource for organic 100% pastured animal products).
7) MACRONUTRIENT RATIOS:
All foods fall into categories called macronutrients: fats, carbohydrates, and proteins. Now that we’ve described some healthful options available to you on this program, you need to be able to put them together in combinations that will promote healing. CRON-O-Meter * is a free online resource that allows you to see the macronutrient (and micronutrient) value of your foods. It can also serve as an online food diary that can help you track and tweak your food intake to reach ketosis by showing you a pie chart of your macronutrient values in real time as they change throughout the day. In general, if you want to create a ketogenic state, you need to reduce your carbohydrates and proteins while increasing your good fats. Within that framework, you can still get enormous amounts of non-starchy vegetables (10+ cups a day) and still achieve ketosis as you are combining diet with other strategies (fasting and exercise) to achieve this goal. You’re not using a ketogenic “diet", as much as you’ll be practicing a ketogenic lifestyle, more reminiscent of healthful, non-Westernized people. As you heal, your protein needs will reduce even further per the guidelines. In contrast to protein and carbohydrate, healthy fat is the one macronutrient that you should enjoy freely. An avocado a day has been shown to reduce LDL particle numbers. Several tablespoons of olive oil can easily be enjoyed with each meal. Olives, nuts and seeds are wonderful accompaniments to salads.
*CRON-O-meter often reports food portions in grams, as opposed to ounces or more traditional units of measurement. A digital scale is very helpful when trying to make that conversion.
To help you visualize what the macronutrient ratios look like for various meals, you can see a few samples below. The first picture shows a sample meal for breaking your fast, typically after noon, but it can be earlier if you are still working on healing from glycotoxicity.

- Four to five cups of organic, non-starchy, preferably seasonal and local vegetables
- Some limited starchy vegetables, sweet potato wedges for beta-carotene, that have been cooked, then cooled to enhance resistant starch
- Pastured eggs that are naturally high in Omega-3s. Notice the yolks are very lightly cooked to preserve the choline, but may be cooked more firmly depending on your preference
- Fermented vegetables
- High polyphenol extra virgin olive oil as a dip for vegetables
- Moderate use of sea salt and other fresh herbs and spices
- Bone broth
Here’s an example for the evening (or second) meal that would typically be eaten at least 3-4 hours before bedtime:

- Five or more cups of organic, non-starchy, preferably local and seasonal vegetables, lightly cooked or raw
- Small serving of wild caught Alaskan sockeye salmon
- Liberal use of healthy fats such as avocado, olives, nuts, seeds & high polyphenol extra virgin olive oil
- Liberal use of seasonings including sea salt, infused vinegars, fresh herbs and spices
Here’s an example of a brain healthy treat. You can make unlimited variations on this crunchy, sweet dessert by swapping out the coconut kefir for an A2 dairy yogurt or flavoring with lime zest, a squeeze of fresh key lime and cinnamon instead of wild berries. A square of dark chocolate (86% or higher cocoa) is another satisfying and healthful treat best enjoyed after a meal to blunt the glycemic response.

- Coconut milk kefir (unsweetened)
- Wild blueberries
- English walnuts
- Sliced Almonds
- Cocoa nibs
- Coconut flakes (unsweetened)
- Sprinkle of stevia
D. GUT HEALTH
Gut health is the foundation of any health program, but is especially critical to brain health. The brain and the gut are intricately and bi-directionally connected. If there are underlying issues with gut health, such as “leaky gut”, SIBO (small intestinal bacterial overgrowth), or H. pylori, you may need additional interventions to aid in the optimization of your nutritional program.
1) Avoid grains and dairy, to the extent possible, as these have been demonstrated to be inflammatory. Grains such as wheat, barley, rye, oats, corn, and soy contain lectins, phytates, and enzyme inhibitors. Lectins (which include gluten) are plant toxins that are “sticky proteins” that create holes in the gut lining (“leaky gut”). The holes in the gut lining allow particles to enter that are seen as foreign, cause inflammation, and can be a set-up for food/allergy intolerances. If the cause of the inflammation is not eliminated, chronic issues may ensue such as autoimmune disease and neurological disease. Pressure cooking does not remove lectins in grains that have gluten such as wheat, rye, barley, and oats. Note that even gluten-free products and flours contain not only lectins, but are also highly processed and high in glycemic load.
Dairy products are inflammatory for several reasons. Dairy in the U.S. comes from a type of cow (A1) that produces an inflammatory lectin-like protein, while A2 cows, sheep and goats do not. For those with gluten intolerance, dairy cross-reacts and mimics gluten.
- Any food allergy/intolerances should be revealed either by testing or elimination. After testing or elimination, any candidate food allergen can be reintroduced, and its effect on your symptoms evaluated (unless there is a severe allergy). Food allergies can be severe and life-threatening, and usually occur closer to the time of ingestion. Food intolerances are usually timed further from ingestion, are less severe and often limited to GI symptoms such as gas, bloating, constipation and/or diarrhea, but can include rashes, arthritis, headaches, fatigue, mood swings irritability and “brain fog”.
- Common food allergies/intolerances besides gluten and dairy are eggs, peanuts, tree nuts, shellfish, soy, nightshades (such as eggplant, tomatoes, hot and sweet peppers, and potatoes), and multiple ingredients/chemicals used in processed foods.
- Other sources of inflammation to gut lining or cause of imbalances are drugs such as antibiotics, anti-inflammatories, PPI (proton pump inhibitors), other medications, GMO foods (which are exposed to glyphophate), alcohol, soft drinks, and, of course, stress.
- If you decide to consider a re-exposure to a food intolerance, wait until you have eliminated that food for 3 weeks to 3 months and determined that your gut has healed, either by blood or stool testing, or a retrial attempt. Keeping a journal of your efforts can be helpful.
2) Incorporate prebiotics and probiotics to help to optimize your microbiome, the bacterial population in your gut. Prioritize real food, over supplemental prebiotics and probiotics. Supplementation provides an important short term fix, while your food changes will create more durable benefits. To reiterate, the brain and the gut are intricately, and bi-directionally, connected. The health of the brain begins with the health of the gut, and gut health begins by promoting a beneficial microbiome.
Prebiotics are foods that are non-digestible by humans, but are digested in the colon by the beneficial bacteria to support their growth, and their by-products support the health of the intestinal lining. Prebiotic foods include the resistant starches and fibrous plants, roots, and tubers. Examples are listed above. Organic psyllium seed husks, acacia fiber, potato, plantain, and green banana starch, inulin, and FOS are examples of supplements that may be helpful. Gradual increases in these prebiotic foods can help mitigate the potential GI side effects.
Probiotic foods contain beneficial bacteria, which convert carbohydrates into lactic acid (i.e., fermentation) and compete with pathogenic bacteria. Probiotic foods include fermented foods such as sauerkraut, kimchi, kombucha, tempeh, miso, and unpasteurized fruits and vegetables pickled in brine. Yogurt or kefir from coconut without added sugar is another option. Proceed cautiously with dairy yogurt or kefir, and only if dairy intolerance is not a problem. Look for unsweetened, full- fat options, made exclusively from grass-fed A2 cows, sheep or goats, although these can be hard to find. Goat milk, which is widely available, is always A2. Strictly avoid dairy from A1 cows.
3) Bone broth can also be useful in healing a “leaky gut.” The bones should come from pastured, organic animals. The bone broth regimen utilizes the collagen of bone to seal the “leaky gut.” There are regimens for multiple gut/neurological and autoimmune diseases that address their reversal primarily through the healing of the gut. Bone broth can be added daily, plain or as a base for soups, stews, and other foods. Kettle and Fire bone broth is one source for organic 100% pastured bone broth.
E. COOKING METHODS
The goal is for the food to taste good, while minimizing the loss of nutrients and the production of AGEs (advanced glycation end products). AGEs are glycotoxins created by a reaction between sugars and proteins or lipids. High levels create oxidative stress, inflammation, and many of the pathologies we see with diabetes and other chronic diseases.
Moist heat, shorter cooking times, lower temperatures, using acidic ingredients such as lemon, lime, and vinegar, and food choices (uncooked plants have no AGEs, uncooked animals do have AGEs) are all methods that reduce AGEs. Grilling, searing, roasting, broiling, and frying will produce AGEs. Avoid non-stick and aluminum cookware due to possible toxicity and metal accumulation. Ceramic and steel cookware are safe choices.
F. IMPLEMENTATION
To learn about your response to your fasting, food, exercise, and sleep, it can be useful to check your glucose and ketones with your present regimen and for the period of time that you transition to a fat-based metabolism.
A Dual Glucose/Ketone Meter can provide you with real time data that can help guide your food choices. It’s a small portable device that allows you to check your glucose and ketones, on disposable strips, by using a prick of blood (obtained by a lancet) from your finger. The Precision Xtra meter, which is widely available, is one example of a dual- purpose meter.
Tracking Glucose gives you information about how your body responds to a given amount of food, especially carbohydrates. A postprandial (after meal) glucose check should be done one and two hours following a meal. It is valuable to see how you respond to your transition period of reducing carbohydrates or the addition of carbohydrates such as resistant starches. Here’s a useful resource with detailed instructions on how to use glucose measurements to aid in your recovery and track your progress.
Tracking Ketones through beta-hydroxybutyrate (BHB), the most abundant ketone found in the blood, is the most accurate and reliable means of measuring levels, especially during the transition to ketosis. (Urine ketosticks and ketone breathalyzers are not recommended for this purpose since they lack specificity and accuracy at very low levels.) Some patients have found that achieving ketosis is very helpful for both healing from glycotoxicity and addressing reduced cerebral glucose utilization. They report cognitive clarity, increased energy, and a stable, calm mood, but this strategy may not be necessary for every patient. Here’s a helpful guide with instructions on how ketone testing can be useful.
Once you’ve made the transition to a fat-based metabolism, this type of testing will no longer be necessary on a regular basis as you will have learned through your testing what it feels like to be in mild ketosis.
___________________
These guidelines should be approved by your doctor, especially if you have an underlying condition such as diabetes or other hormonal condition, cardiovascular disease or hypercholesterolemia, cancer, or you are malnourished, underweight or suffering from an eating disorder. You may also consider that diabetics and those with cardiovascular disease or hypercholesterolemia have shown remarkable benefits from a ketogenic lifestyle, but have to monitor their symptoms and biomarkers carefully as their dosage/need for medications will be affected. Cancer patients have also been shown to benefit from a ketogenic lifestyle as cancer cells require glucose for their metabolism, therefore cancer cell growth may be inhibited.
Keep Your Blood Sugar Safe
First Step: Know Your Blood Sugar!
Tracking your blood glucose is an empowering first step towards gathering data that can help you get onboard the Bredesen Protocol and adopt a Ketoflex 12/3 lifestyle. You can purchase a glucometer (glucose meter) at any pharmacy, but we recommend that you use a dual glucose/ketone meter that can provide you with real time data that can help guide your food choices. It’s a small portable device that allows you to check your glucose and ketones, on disposable strips, by using a single drop of blood (obtained by a lancet) from your finger. It’s important to use a meter that is accurate at measuring low levels of beta-hydroxybutyrate (BHB), a type of ketone body. (Urine ketone strips are generally too imprecise at lower levels to be helpful.) The Precision Xtra and Keto-Mojo systems are two examples of this kind of dual-purpose meter.
Tracking glucose gives you valuable information about how your body responds to a given amount of food, especially carbohydrates. A post-prandial (after meal) glucose check might also be helpful one and two hours following a meal, depending upon your fasting glucose level. It is valuable to see how you respond to your transition period of reducing simple carbohydrates like sugar or high-fructose corn syrup, or adding lower glycemic carbohydrates such as resistant starches. Below is a useful resource with detailed instructions on how to use glucose measurements to aid in your recovery and track your progress. Once you’ve successfully made the transition to a fat-based metabolism, this type of testing will no longer be necessary on a regular basis, since you will have learned, through your testing, what it feels like to have achieved mild ketosis.
How to use your Glucose Measurements to Guide your Recovery
Consider keeping a journal of your blood glucose measurements so that you can track your progress. Measuring your glucose provides you real time data to track how your body is responding to a given food or meal.
Always follow the manufacturer’s instructions for how to perform a glucose test. Glucose testing strips are inexpensive and widely available.
It’s helpful to test fasting morning glucose before coffee, supplements or medications. Your goal is a reading between 70-90 mg/dL (3.89–5.00 mmol/L.)
If your reading is within that range, you are likely insulin sensitive. You needn’t perform post-prandial (after meal) checks at every meal unless you want to check your response to a specific food. Continue testing fasting morning blood glucose for a week or two to see if you stay in the optimal range of 70-90 mg/dl. If you have occasional lapses, move on to post-prandial checks.
If your reading is higher than the recommended range, it’s a good idea for you to perform regular post-prandial checks one and two hours after each meal so that you can identify the foods that are causing your glucose spikes, and make adjustments to your diet.
A post-prandial test is typically performed twice after finishing a meal; at one hour, then at two hours. Some people experience delayed glucose elevation, so be sure to do the second test even if the first one is within range.
1) One hour after finishing a meal, your blood glucose should be between 90–125 mg/dL (5.00–6.94 mmol/L.) 2) Two hours after a meal, your goal is 90–110 mg/dL (5.00–6.11 mmol/L.) 3) Five hours after a typical meal, your blood glucose should return to the fasting range, ideally between 70–90 mg/dL (3.89–5.00 mmol/L.)
If your readings are higher than the stated goals, you need to identify the foods that are causing the hyperglycemic response. Obvious culprits are anything with sugar or fructose, even "healthy" sweets like fruit (especially tropical fruits like pineapple), honey, or maple syrup. Starchy carbohydrates like white potatoes, rice, oats, pasta, or bread are other common triggers. Even sweet potatoes can cause a spike; hence they are only recommended in small quantities. Other typical culprits are resistant starches, legumes, and quinoa. Additionally, excess protein can also contribute to higher readings.
Try replacing the suspected trigger with healthy fats (EVOO, olives, avocados, nuts, and seeds) and/or non-starchy vegetables at your next meal. See our Nutritional Guidelines for greater detail. Repeat your post-prandial testing and journal your body’s response.
Continue this process for every meal until your fasting morning glucose falls within range.
Cooking, then cooling, resistant starches (see our Nutritional Guidelines for a description of resistant starches) increases their resistant starch level, and may reduce their glycemic load. Test your blood sugar to gauge your response. Some people still can’t tolerate these carbohydrates even if they’ve been previously cooled.
Be aware that everyone, based on genetics, general state of health, gut microbiome status, stress levels, and myriad other factors has a different glycemic response to the same food. You may even have a high degree of variable responses to the same food due to extraneous contributors, such as stress, poor sleep, hormone status, and multiple other factors. Identifying and addressing your triggers will help you to heal.
Understand that once you’ve keto-adapted (switched from burning primarily glucose to fat) your fasting morning glucose may rise a bit over time (this may be because the low level of insulin is no longer enough to shut down the liver’s production of glucose), but should still remain in the optimal range of 70-90mg/dL. Concurrently checking ketones can offer you reassurance. Their presence (>0.5mmol/L) indicates that this rise is likely of little consequence, especially if your HgbA1c (hemoglobin A1c) and fasting insulin levels remain within the optimal range (hemoglobin A1c <5.4%, and fasting insulin <5mIU/L).
After you’ve been keto-adapted for weeks or months, if you experience an inexplicable, dramatic rise in fasting blood glucose, it may be a sign that you need to periodically (weekly or bi-weekly) transition to a glucose-burning state for a short time by adding more approved carbohydrates so that your body maintains metabolic flexibility. The ability to seamlessly transition back and forth from a glucose-based fuel to a fat-based fuel is a sign of optimal health. You may notice a cognitive fogginess that accompanies this transition out of ketosis. Be sure to track this cognitive change in your journal and switch back to your typical ketogenic diet at your next meal.
Be aware that your blood glucose may temporarily be elevated following exercise. Your liver responds to the energy demands of exercise by releasing more glucose. This is typically inconsequential and will quickly drop down to your pre-exercise level or even lower.
Source of good fats

Olive Oil — One Source of Good Fats
Olive oil, as noted in the Nutrition Guidelines, is an important part of the Ketoflex 12/3 Diet for many reasons. Olive oil consumption contributes to improved cognition, helps to yield healthy cholesterol results, and is inversely correlated with beta-amyloid. Sourcing the right olive oil, however, is tricky and requires many considerations.
First, look for extra virgin olive oil (EVOO). Pure olive oil is a lower-quality, refined oil, with a lighter color, and a more neutral flavor. EVOO is always unrefined, and free from any chemical treatment. It has a stronger flavor and is superior in its health benefits.
Always look for a brand that provides the harvest date to ensure that you’re getting the most recent date available. Avoid brands that don’t list this information. After sitting on a shelf, the polyphenol content of even the best EVOO is reduced. There are many different EVOO varieties from all over the world, each with a different harvest time.
Your next consideration is the polyphenol content. You want the highest polyphenol content possible. Polyphenols have major antioxidant and anti-inflammatory properties that provide protection from oxidative stress.
- Be aware that polyphenols are also responsible for the bitter taste of EVOO. It takes time to acclimate to the higher polyphenol varieties, especially if you are used to grocery store brands. You may want to transition slowly to a variety with a 300+ count before moving onto the higher 500+ options.
- Always look for a glass bottle that is dark in color to protect the oil from oxidation that naturally occurs with light exposure.
- Never buy EVOO that is in a plastic bottle. Toxic chemicals from the plastic may leach into the EVOO.
- Be aware that many grocery store varieties of EVOO are actually blends of many different oils, not pure EVOO.
- Store EVOO in a dark cool place in your home. Only buy as much as you can comfortably use in a several month period. Freezing or refrigerating olive oil destroys some of the healthful properties.
Olive oil 100
EVOO is best used as a finishing oil for salads or cooked vegetables. You can make excellent dressings or sauces that actually increase the bioavailability of nutrients in the vegetables.
It’s acceptable to cook with higher polyphenol varieties on very low heat (but not high heat—EVOO is damaged by high heat), with the understanding that the polyphenol level will be reduced by exposure to heat. A small splash of high polyphenol EVOO used with ceramic or other safe cookware on low to medium heat is fine for sautéing. You can also roast vegetables splashed with a small amount of high polyphenol EVOO roasted at temperatures below 350 degrees Fahrenheit. Freely season and finish both with additional amounts of EVOO to enhance flavor and add healthful polyphenol benefits.
One excellent source for healthful EVOO is Amphora Nueva. While their website is educational, it’s best to call (925) 310-4681 directly to place an order, to ensure that you’re getting the highest polyphenol count, since they continually source oils from all over the world. They offer inexpensive shipping all over the continental United States.
People often ask how much EVOO they should be using. If your goal is to be in ketosis, many participants find it helpful to get approximately 70% of their calories from fat. By using CHRON-O-meter, you can determine how much fat you’re getting from other sources like nuts, seeds, olives, avocados, fatty fish, etc. to best make this determination. In general, feel free to use this healthful oil liberally as an important and healthful ingredient in your diet.
Mixing EVOO with an acid such as that from naturally flavored vinegars or the juice of citrus fruits (keeping the glycemic index low), mixed with fresh herbs and seasonings, brings your salads and vegetables to life. For a twist, you can try a salad dressing with a Middle Eastern flair by combining 1/2 cup of EVOO with 2 TBS of tahini and the juice of a whole lemon. Add fresh minced garlic, pink Himalayan salt, cracked pepper and cumin to taste, and whisk to blend.
EVOO can also be used to make fresh homemade garlic aioli that’s an excellent accompaniment or dip for any vegetable. Start by grinding several cloves of garlic with a mortar and pestle. Once ground, transfer to a tall cylindrical container. Add one cup of EVOO, a fresh pastured egg (wash the shell first), the juice of 1/2 lemon, and a dash of salt. Place your immersion blender all the way to the bottom of the container and whisk for 30 seconds. Voila’, you’ve created a healthful, delicious aioli. Play with different herbs and seasonings for variety.
MCT OIL
Medium-chain triglycerides (MCTs) are a naturally occurring source of dietary fats that are abundant in coconut oil. Our bodies rapidly convert them into ketones, which can be used as an energy source by the brain. No studies have yet found that MCTs can prevent dementia, but some evidence suggests that patients with dementia might find short-term benefit using MCTs. While they are generally considered safe, some gastrointestinal side effects are common.
Two clinical trials reported that MCT supplements improved cognitive function in mild cognitive impairment (MCI) and Alzheimer's disease patients who do not carry the APOE4 genotype but were ineffective for APOE4 carriers.
Two clinical trials suggest that an MCT supplement (Axona®) may provide an acute benefit in patients with MCI and Alzheimer's disease. However, these improvements were short-lived and disappeared 14 days after the supplement was stopped. Both trials were funded by Accera, the company that sells Axona®. No studies have tested the effects of MCTs in patients with severe dementia.
Strong evidence suggests that MCTs are low risk when used by healthy adults. Foods high in MCTs such as coconut oil are used widely with few adverse events reported. For some people, though, MCTs can increase plasma triglyceride levels, which might be harmful for cardiovascular health. And mild gastrointestinal side effects are common in individuals taking MCTs. The side effects may be reduced by taking MCTs with food and by slowly incorporating them into the diet.
- Cunnane SC, Courchesne-Loyer A, St-Pierre V et al. (2016) Can ketones compensate for deteriorating brain glucose uptake during aging? Implications for the risk and treatment of Alzheimer's disease . Annals of the New York Academy of Sciences 1367, 12-20.
- Castellano CA, Nugent S, Paquet N et al. (2015) Lower brain 18F-fluorodeoxyglucose uptake but normal 11C-acetoacetate metabolism in mild Alzheimer's disease dementia . Journal of Alzheimer's disease : JAD 43, 1343-1353.
- Page KA, Williamson A, Yu N et al. (2009) Medium-chain fatty acids improve cognitive function in intensively treated type 1 diabetic patients and support in vitro synaptic transmission during acute hypoglycemia . Diabetes 58, 1237-1244.
- Pan Y, Larson B, Araujo JA et al. (2010) Dietary supplementation with medium-chain TAG has long-lasting cognition-enhancing effects in aged dogs . The British journal of nutrition 103, 1746-1754.
- Kashiwaya Y, Bergman C, Lee JH et al. (2013) A ketone ester diet exhibits anxiolytic and cognition-sparing properties, and lessens amyloid and tau pathologies in a mouse model of Alzheimer's disease . Neurobiology of aging 34, 1530-1539.
- Henderson ST, Vogel JL, Barr LJ et al. (2009) Study of the ketogenic agent AC-1202 in mild to moderate Alzheimer's disease: a randomized, double-blind, placebo-controlled, multicenter trial . Nutrition & metabolism 6, 31.
- Reger MA, Henderson ST, Hale C et al. (2004) Effects of beta-hydroxybutyrate on cognition in memory-impaired adults . Neurobiology of aging 25, 311-314.
- Yin JX, Maalouf M, Han P et al. (2016) Ketones block amyloid entry and improve cognition in an Alzheimer's model . Neurobiology of aging 39, 25-37.
- Nosaka N, Kasai M, Nakamura M et al. (2002) Effects of dietary medium-chain triacylglycerols on serum lipoproteins and biochemical parameters in healthy men . Biosci Biotechnol Biochem 66, 1713-1718.
- USE OF MEDIUM CHAIN TRIGLYCERIDES (MCT) IN ALZHEIMER’S DISEASE (AD): PILOT TRIAL.(2017). Janak NathanEmail the author Janak Nathan, Siddika Panjwani. P2-020. DOI: https://doi.org/10.1016/j.jalz...
High Quality MCT Oil Brands
CLICK ON THE ICON TO ORDER
To Order Discounted High Quality MCT Oil From Wellevate ask Dr. Sadak for a recommendation and log in to your account to place an order.

Glucose recover guide
How to use your Glucose Measurements to Guide your Recovery 04/08/18
Consider keeping a journal of your blood glucose measurements so that you can track your progress. Measuring your glucose provides you real time data to track how your body is responding to a given food or meal.
Always follow manufacturer’s instructions for how to perform a glucose test. Glucose testing strips are inexpensive and widely available.
It’s helpful to test fasting morning glucose before coffee, supplements or medications. Your goal is a reading between 70-90 mg/dL (3.89–5.00 mmol/L.)
If your reading is within that range, you are likely insulin sensitive. You needn’t perform post-prandial (after meal) checks at every meal unless you want to check your response to a specific food. Continue testing fasting morning blood glucose for a week or two to see if you continuously stay in range. If you have occasional lapses, move on to post-prandial checks.
If your reading is higher than the recommended range, it’s a good idea for you to perform regular post-prandial checks after each meal so that you can identify the foods that are causing your glucose spikes and make adjustments to your diet.
A post-prandial test is typically performed twice after finishing a meal; at one hour, then at two hours. Some people experience delayed glucose elevation, so be sure to do the second test even if the first one is within range.
One hour after finishing a meal, your blood glucose should be between 90–125 mg/dL (5.00–6.94 mmol/L.) Two hours after a meal, your goal is 90–110 mg/dL (5.00–6.11 mmol/L.)Five hours after a typical meal, your blood glucose should return to the fasted range between 70–90 mg/dL (3.89–5.00 mmol/L.)
If your readings are higher than the stated goals, you need to identify the foods that are causing the hyperglycemic response. Obvious culprits are anything with sugar or fructose, even “healthy” sweets like fruit, honey, or maple syrup. Starchy carbohydrates like white potatoes, rice, oats, pasta, bread are other common triggers. Even sweet potatoes can cause a spike, hence they are only recommended in small quantities. Other typical culprits are resistant starches, legumes, and quinoa. Additionally, the macronutrient context of your meal can contribute to higher readings. Protein or carbohydrates in excess should be suspected.
Try replacing the suspected trigger with healthy fats (EVOO, olives, avocados, nuts, and seeds) or non-starchy vegetables at your next meal. See our Nutrition Guidelines for greater detail. Repeat your post-prandial testing and journal your body’s response.
Continue this process for every meal until your fasting morning glucose falls within range.
Cooking, then cooling, resistant starches (that are typically cooked) increases their resistant starch level and may reduce their glycemic load. Test your blood sugar to gauge your response. Some people still can’t tolerate these higher glycemic foods even if they’ve been previously cooled.
Be aware that everyone, based on genetics, general state of health, gut microbiome status, stress levels, and myriad other factors has a different glycemic response to the same food. You may even have a high degree of variable responses to the same food due to extraneous contributors, such as stress, poor sleep, hormone status, and multiple other factors. Identifying and addressing your triggers will help you to heal.
Understand that once you’ve keto-adapted (switched from burning primarily glucose to fat) your fasting morning glucose may rise a bit over time. Concurrently checking ketones can offer you reassurance. Their presence (>0.5mmol/L) indicates that this is likely of little consequence especially if your HbA1c and fasting insulin levels remain within range.
After you’ve been keto-adapted for weeks or months, if you experience an inexplicable, dramatic rise in blood glucose, it may be a sign that you need to periodically (weekly, bi-weekly, monthly?) transition to a glucose-burning state for a short time by adding more approved carbohydrates so that your body maintains metabolic flexibility. The ability to seamlessly transition back and forth from a glucose-based fuel to a fat-based fuel is a sign of optimal health. You may notice a cognitive fogginess that accompanies this transition out of ketosis. Be sure to track this cognitive change in your journal and switch back to your typical ketogenic diet at your next meal.
Be aware that your blood glucose may temporarily be elevated following exercise. Your liver responds to the energy demands of exercise by releasing more glucose. This is typically inconsequential and will quickly drop down to your pre-exercise level or even lower.
Exercise — Yes, It Really Helps!
From among all of the various strategies outlined in the ReCODE protocol, none has more scientific evidence than exercise. By far, exercise is the single most important strategy you can employ, both to prevent and remediate cognitive decline. Exercise is beneficial in many ways. It can help maintain a healthy Body Mass Index (BMI), reduce insulin resistance, reduce inflammation, improve blood pressure, and reduce the risk for heart disease and stroke. It also reduces stress and anxiety, while improving mood and sleep.
Everyone wants to know the best form of exercise for brain health. Research is mixed, with aerobic exercise taking a slight lead over strengthening exercise, but both are vitally important especially as we age, especially since the two different types of exercise activate different mechanisms, thus inhibiting cognitive decline by different routes. HIIT (high-intensity interval training) has also been shown to be beneficial for cognition, especially processing speed (effects of three exercise modalities), but if you do HIIT, please make sure not to ramp up so quickly that you put yourself at risk for a heart attack.
Aerobic exercise is thought to be beneficial by several mechanisms. It increases blood flow and powerfully upregulates brain-derived neurotrophic factor (BDNF), an important protein that stimulates production of new brain cells and strengthens existing ones. Older adults with higher cardiorespiratory fitness also have better preservation of overall brain volume, increased cortical thickness, and greater white matter integrity, leading to higher levels of executive function, critical thinking, and planning skills.
Strength training prevents sarcopenia, the loss of lean muscle mass that occurs with aging. Sarcopenia is strongly correlated with cognitive decline. Strength training also prevents loss of bone, improves brain function, slows aging, and prevents brain atrophy. Adults who strength train have enhanced long term memory, fewer white matter lesions in the brain, an improved gait, and can more easily perform daily tasks of living. An interesting study focusing on muscles in the legs demonstrated that leg power reliably predicted both cognitive aging and global brain structure.
One of the best forms of aerobic exercise, one that incorporates strength training because it’s a naturally weight bearing exercise, is walking. Try to incorporate a daily walk into your routine. Depending on your current fitness level, you may need to start slowly. That’s okay. Always walk with a purpose, increasing the length of your walk by a few minutes a day until you reach 30 minutes or more. Consider the strategies below to enhance your walk:
RETHINK EXERCISE. Rather than viewing it as an obligation, make it the highlight of your day. It’s your dedicated time to simply move and exquisitely care for yourself. You’re worth it. Make it joyful. Keep it fun.
GET OUTSIDE. Research shows that spending time in nature is good for your brain. It’s been scientifically proven to boost creativity, problem-solving skills, sharpen mental focus and minimize rumination. The beauty of nature also instills you with a sense of wonder that translates to better connectedness and compassion towards others.
WALK WITH A FRIEND. Connecting with others is vital for brain health. Consider walking with a friend or family member so that you can socialize as you exercise.
PLAY WITH SPEED. As you feel stronger on your daily walk, consider increasing speed and even adding short periods of jogging or sprinting.
ADD MUSIC. When walking alone, listen to your favorite music and even sing along. You could also listen to meditative music, to unwind as you walk.
BRAIN TRAIN. Incorporate cognitive training into your daily walk. Practice saying the alphabet backwards. You could even try counting backwards from 100 by 5s, 6s, 7s, 8s, and 9s.
MIX IT UP. Great alternatives to walking include cycling and even cross-country skiing in the winter. If you live near a body of water, you might consider kayaking for a terrific upper body workout.
TRACK YOUR PROGRESS. Consider using a non-Wi-Fi pedometer-tracking device to monitor how much you’re moving. For a realistic goal, start working towards 10,000 steps per day. Keep a journal to note how exercise is changing the way you feel, look, and affecting your cognition.
Having dedicated daily exercise time set aside is vital, but it’s even better to try to increase movement all throughout the day. Look for hidden opportunities in your daily schedule. Purposefully park your car far away from your destination so that you can incorporate a long walk while running your errands. Whenever you have the opportunity to take an elevator or escalator, take the stairs instead. Reframe the way you look at your household chores. Rather than feeling overwhelmed by them, think of them as opportunities for increasing your activity level. Especially embrace your chores in the yard. Pulling weeds, spreading mulch, sweeping, raking, or shoveling snow all keep you active and make you stronger. Even household chores like carrying laundry up and down the stairs, bending over to clean baseboards, or mopping the floor help to keep your muscles strong.
Given the importance of building leg strength, you may want to include daily squats into your exercise routine. If your leg muscles are weak, you can start by standing in front of a chair as if you were going to sit down. Move your buttocks towards the seat and hold that position right above the chair as long as possible. You should feel a burn in your thigh muscles called quadriceps. It’s okay to fall into the seat if you feel the need. That’s why you’re starting in front of a chair. Try to resume standing and repeat for several repetitions. Over time, your leg muscles will get stronger.
Consider joining a local gym, YMCA, senior or community center for group strengthening classes or to work with a trainer to develop a program to meet your goals. It’s often more enjoyable to train while benefiting from a supportive relationship or spirited group atmosphere. If you’re recovering from an injury or have a condition that limits your mobility, look for seated exercise classes. These specially-designed chair workouts can offer decent exercise within a wide range of abilities.
Yoga and Pilates also offer excellent strength training workouts ideal for everyone, but are especially good for anyone dealing with mobility issues. This type of workout can also be incorporated into your meditation practice, and help to increase your balance and flexibility, both of which are vital as you age.
If you’ve previously been sedentary, it may be difficult to get started, but the daily practice of exercise becomes self-sustaining over time. Baby steps turn into exhilarating hikes through nature. The more you exercise, the better you’ll feel, and the more you’ll want to exercise. When starting any exercise program, be sure to check with your physician to make sure that you’re healthy enough to engage in your preferred activity. It’s always tempting to overdo, but you ultimately hurt yourself if you sustain an injury and have to refrain from exercise while you heal.
Get out there. Make a daily appointment with yourself. Keep it joyful and fun. Your exercise time should be the highlight of your day. Additionally, keep moving throughout the day for optimal health. Daily exercise is the single most effective strategy in your cognitive repair kit.
The Many Benefits of Optimal Sleep
An explosion of scientific discovery in the last twenty years has shed new light on the fundamental role of sleep on our cognition and overall wellbeing. Sleep enriches our ability to focus, learn, memorize, and make logical decisions, and is critical for everyone at all stages of life. A lack of sleep affects overall health and leads to obesity, diabetes, heart disease, and a weakened immune system. All of these conditions impact brain health.
One of the most vital roles of sleep is to help us solidify and consolidate memories. As we go about our day, our brains take in an incredible amount of information. Rather than being directly logged and recorded, however, these facts and experiences first need to be processed and stored; and many of these steps happen while we sleep. Overnight, bits and pieces of information are transferred from more tentative, short-term memory to stronger, long-term memory—a process called "consolidation." Too little or disturbed sleep has profound implications on many aspects of cognition, including our ability to focus, learn, form memories, and execute effective decision making.



We know that sleep loss and depression are also intertwined. People who are depressed often have trouble sleeping (or they’ll sleep in excess), but they’ll also have other symptoms that suggest depression may be driving the process. A sense of pervasive sadness, a loss of interest in old hobbies, a change in appetite, a loss of energy, and trouble concentrating are tip-offs that you may be dealing with depression. If you feel this may be an issue for you, have a discussion with your functional medicine practitioner. For many, improving sleep quality and quantity may help with depression.
Sleep apnea, a brief period of breathing cessation, is emerging as an important risk factor for Alzheimer’s disease. If you or your loved one snores, you need to rule this out. You can start with a home pulse oximeter to check to see if you’re getting too little oxygen throughout the night. If this appears to be a problem, arrange for a formal sleep study through your physician. While it’s somewhat inconvenient as you often have to sleep in a controlled setting, it’s typically covered by insurance and will determine the necessity of a breathing machine called a CPAP that can treat this condition.
Sleep medication might temporarily help, but in the long run benzodiazepines andanticholinergic medications increase your risk for cognitive decline. Luckily, there are several medications and supplements that are neuroprotective and naturally sedative. Many people are deficient in magnesium, a mineral necessary for hundreds of biochemical reactions in the body. Magnesium has sedative properties and can be taken before bed to help you relax. Melatonin, which naturally decreases with age, can be supplemented to create natural physiological sleep. Ashwaghanda and Bacopa monnieri, both adaptogens, have sedative effects for many people. If you wake up in the middle of the night, tryptophan may be helpful. Many women, who use bHRT as a part of their protocol report improved sleep. If these have been recommended as a part of your ReCODE protocol, experiment to see the effect they have on your sleep. Be sure to trial one at a time and carefully journal the effect. Be aware that if you decide to layer several supplements at once, you may get a different effect. Tweak until you find a combination that’s helpful.
While much of the biological necessity of sleep remains a mystery, some exciting new scientific research is revealing that our brain engages in vital restoration work as we sleep. Scientists have recently discovered a system that drains waste from our brains called the glymphatic system. Research reveals that it functions most effectively during sleep allowing it to clear a toxic protein called beta-amyloid, the accumulation of which is correlated with Alzheimer’s disease. A recent study reveals that even one night of sleep deprivation had a profound impact on beta-amyloid clearance.
Great sleep doesn’t just happen in the same way that a great walk doesn’t just happen. Both are natural physiological functions yet still involve some degree of preparation and planning to be successful. Think about it. Before you go out for a walk, you check the weather and make sure that you’re dressed appropriately. You go to the bathroom beforehand, so you won’t be caught in the middle of your walk. You ensure that you’re hydrated and even carry water if it’s warm outside. You chose the right footwear for the weather and conditions. You carefully adjust your socks, so you won’t get a blister and lace your shoes to ensure they remain snug for the duration of your walk. You charge your iPod, find your earbuds, and choose your music to suit your mood. You might coordinate to walk with a friend and settle on a time and meetup spot, etc. The list, while instinctive, is extensive.

Too many people mistakenly assume that you can just lie down, and you’ll fall asleep. That’s sadly not true for many of us and this issue tends to worsen as we grow older. You need to put a similar amount of attention and preparation into your nightly sleep hygiene. The great news is that we can work to optimize sleep.Applying the strategies below will help improve both the quality and quantity of your sleep.
- Try to stick to a regular sleep schedule. It’s not always possible because of family or work demands but do your best to have a regular bed and waking time. Ideally, we should begin to wind down as the sun is setting.
- Make seven to eight hours of sleep your goal. Research shows that people getting less than six hours and more than nine hours are negatively impacted.
- No caffeine (or other stimulating beverages or supplements) past the early afternoon. Work to identify which supplements are stimulating and be sure to include them in your morning stack.
- Eat your last meal of the day at least 3 hours before bed. This promotes autophagy which cleans out cellular waste products. It’s also much easier to sleep on an empty stomach.
- If you’re struggling with sleep, refrain from alcohol. The sedative effect of alcohol may seem to help with sleep, but research shows that it actually disrupts circadian rhythm and sleep-wake cycles leading to disrupted sleep.
- Don’t exercise within three hours of bedtime. Exercise ramps up adrenaline and prevents sleep.
- Take your supplements a few hours before bed with as little water as possible. While it’s important to hydrate during the day, you don’t want to have to wake up for a bathroom run.
- Refrain from stimulating activities or conversations several hours before you plan to sleep.
- Wear your blue blocking glasses three hours before bedtime. Read more about how they work here .
- Make your bedroom your sanctuary. Keep it clean, uncluttered, free from work and any other projects.
- Sleep alone if you know you’ll be interrupted at night. This is especially important if you and your partner have different sleep habits due to work or other demands.
- No TV in the bedroom.
- Minimize Wi-Fi. Mounting evidence suggests that it can negatively impact overall health. Make sure any electronic device in your room is turned off or to airplane mode when you go to sleep.
- Switch to an eBook if you read before bed. Make sure to pick one that lights up (so you don’t need a lamp) with blue blocking features that automatically turns off.
- Completely darken the bedroom or use a sleep mask. Any small bit of light at night will interfere with melatonin production.
- Keep the bedroom cool. Research shows that keeping the temperature between 60-67 degrees Fahrenheit depending upon your preference, is optimal for sleep. If you tend to be cold, be sure to have a warm blanket to cover up with.
- Try a weighted blanket. In the same way that babies, who are swaddled sleep more deeply, some adults report a similar effect with a weighted blanket. This strategy is most effective for those who struggle to stay warm. Experiment to see if this is helpful for you.
- Use a white noise machine if you’re regularly interrupted with extraneous noise from your heating system, air conditioner, outside traffic, neighbors, etc. Many have relaxing nature sounds (like rain, wind, or waves) that you can set to your desired volume to drown out bothersome noise. Be sure to place this as far from the bed as possible (with the volume optimized) to protect yourself from electromagnetic radiation.
- Consider aromatherapy. Lavender essential oils have proven helpful in slowing heartbeat, relaxing muscles, and promoting slow wave sleep. Put a few drops on a cotton ball near your bed to see how it affects you.
What if you wake up in the middle of the night with stress or anxiety? If you find that you’re mulling over a negative event in the past or feeling stressed about a future event, try a sensory mindfulness technique. Begin by simply focusing on the gentle natural rhythm of your breathing. Slowly breathe in and out. Gradually transition to focus on each of your five senses simultaneously. Feel the soft blankets against your skin, smell the lavender, listen to the sound of your breath, look at the subtle images behind your closed eyes, and taste the clean residue from your brushed teeth. By being fully present -not thinking about the past or future- you can relax and feel safe. With practice this can be very relaxing and help you drift off to sleep. Regular daily meditation, with the last practice before the final meal of the day, can also be very helpful in optimizing sleep.
Thankfully, poor sleep is a modifiable risk factor. By regularly employing all of these sleep optimization strategies, you can make bedtime a nightly ritual that you actually anticipate for the relaxation experience. Improving sleep quality will also offer almost immediate benefits to your mood and overall cognitive performance.
Improve Sleep by Reducing Blue Light
Want to get the inside scoop on a sleep hack that will enable you to make your own melatonin? Blue blocker glasses, with designer options, are all the craze with lots of Hollywood celebs because they work. More and more people are donning these crazy looking orange colored glasses several hours before bedtime to get the best sleep ever.
Let’s dive into the science behind the trend. It has to do with a mismatch between modern civilization and our primitive biology. For hundreds of thousands of years, mankind awoke with the sun and fell asleep when it set. With the advent of fire, early man may have sat around a communal wood-fueled bonfire for warmth and protection from animals, but even that light provided a gentle orange-red glow. Fast forward to modern life, where people work around the clock. Florescent, LED, and incandescent lighting twenty-four hours a day makes that possible, but also throws our natural circadian rhythm (also known as our sleep-wake cycle) into a tizzy. Even worse is the strong blue light that comes from our electronic devices and televisions, especially right before we go to sleep.
Nature prepared us for sleep beautifully with gradual darkness, which automatically signals our pineal gland to naturally produce melatonin necessary for falling and staying asleep. With indoor lighting and multiple electronic devices emitting blue light that mimics daytime, our pineal glands are confused at best- dramatically underproducing this essential hormone that we need for sleep and more. Melatonin is also a powerful free-radical scavenger and wide- spectrum antioxidant protecting against mitochondrial oxidative stress while providing immunological benefits. Production naturally falls off as we age, but with some hacking you can increase beneficial levels.
Blue blockers1@2x 100
Consumer groups have found that inexpensive versions of these glasses are just as effective as pricier designer options. Be sure to look for orange tinted glasses (not medium or light yellow) designed to promote sleep. There are styles specifically geared for those who wear glasses beneath your blue blockers. See tips below to maximize effectiveness:
Wear them regularly, that is, each night if possible. They don’t work like a sleeping pill, but over time they will naturally induce restorative physiological sleep by increasing your own production of melatonin.
If you already are supplementing with melatonin, you may have to decrease your dosage over time, since the blue blockers will be increasing your own production of melatonin.
Put them on approximately three hours before bed. You can easily wear them around the house, or they can serve as a hip conversational topic when you wear them to evening engagements.
Choose a style that blocks all blue light. Wrap-around versions are especially effective and specific styles can accommodate glasses beneath.
Unless your bathroom is equipped with dim blue-blocking light (which is easy to do with a small lamp), be sure to perform any nightly face washing ritual before donning your glasses. Otherwise, you’ll be briefly exposed to harsh blue light right before you go to bed.
Even with blue blockers on, try to minimize exposure to electronic devices right before bed. Engage in other relaxing activities such as quiet conversation or reading.
Once you’re ready for sleep, ensure that your bedroom is 100% dark or wear a sleeping mask to maintain the beneficial melatonin effect.
If you enjoy reading before bed, use a dimly lit blue-blocking electronic device with an automatic shut-off on airplane mode in a dark room. This prevents the necessity of a bedside lamp.
Once you awaken in the morning, open your blinds to the full extent. Better yet, get outside as soon as possible. Exposing your eyes to blue light, especially in the morning, will help get your circadian rhythm back on track.
Improving Sleep by Daily Tracking and Monitoring.
Sleep Coaching. Oura Ring. For more information click Here.
The Perfect Night’s Sleep Formula
Let’s put everything together to create the perfect sleep formula. I know it’s summer and the days are longer, and not everyone has the same schedule but remember this is a guide to help you create your ownperfect sleep formula.
5:00 am – Wake up before the sun rises (or at least 15 minutes then your usual time, to get the first win of the day)
5:05 am – Start your day with a routine to success
5:45 am – Get some exposure to red light from rising sun
7:00 am – Do some aerobic type of activity
12:00 pm – Lunch break, try to go outside or close to a window where you can get some sun exposure
4:00 pm – Last cup of coffee for the day
5:00 pm – Strength training workout
6:30 pm – No blue light, (use the glasses for TV or computer, or dim the lights down in the house)
7:00 pm – Dinner time, try to eat protein that has high tryptophan levels
8:30 pm – Passion flower tea with a touch of honey
9:00 pm – Prepare for bed, make your bedroom cold and dark.
9:01 pm – Turn your phone off or to airplane mode, if you feeling frisky now is the time for the big O.
9:30 pm – Start some meditation and breathing techniques, and slowly drift to better sleep.
(Kevin Masson MS, CSCS, NSCA-CPT, USAW)
Brain Training. BrainHQ. brainhq.com

AHNP and ReCODE uses the BrainHQ exercises and assessments as part of The Bredesen Protocol. BrainHQ is an online (and in app) platform that includes dozens of exercises targeted at specific cognitive skills. It has been developed, tested, refined and validated by a global team of hundreds of brain scientists.
RECOMMENDED USAGE
We recommend training for 20-30 minutes per day, at least three days per work. Training for more days is better. You should pick a time of day when you usually feel most alert, and find a quiet place to train.
PROGRESS
The exercises will quickly and continuously personalize to you, based on all prior responses. They are designed to continuously push you just beyond your prior capabilities. You can track usage and progress through the “Progress” tab at the logged-in home screen. Sleep helps consolidate gains, so what seems hard today may seem easy tomorrow. Please explore and enjoy BrainHQ.
BRAINHQ STUDIES AND BENEFITS
More than 100 peer-reviewed studies show BrainHQ assessments and exercises deliver benefits across various populations. Studies show BrainHQ exercises drive significant improvements in older adults in standard and real world measures of:
Cognition (eg, processing speed, attention, memory, executive function)
Quality of Life (eg, mood, confidence, self-rated health, health-related quality of life)
Real World Activities (eg, movement, balance, driving, functional independence)
Copyright © 2019, AHNP Health
GROUND ZERO: Is My Brain Getting Enough Oxygen?
A = Airway : Is anything obstructing your airway, either during the day or at night?
B = Breathing : Are you breathing deeply and easily (preferably through your nose) without discomfort?
C = Circulation : Is your cardiovascular system healthy and continuously pumping and delivering oxygen to your brain and your body?
We'll take a deeper dive into each and discuss ways to optimize oxygen saturation (the amount of oxygen in your blood) to maximize oxygen delivery to your brain. We'll also discuss ways you can actually monitor your oxygen so that you'll know where you stand. Your goal is to have high levels both during the day and at night. This is measured as a percentage. Healthy people typically have oxygen saturation between 96-99%. During the night, your goal is to maintain oxygen levels around 95-98%, ideally as close to your daytime levels as possible. If you live at a higher altitude, this will drop accordingly. For instance, healthy individuals who live 1,600 meters above sea level (one mile) will typically have oxygen saturation levels above 92%. For those who are acclimated to lower levels, this shouldn't pose a problem. Those with cognitive decline who are not acclimated to higher elevations may want to reconsider traveling to such areas until the cognitive decline has been treated optimally.
Airway
Many people experience partial airway obstruction during sleep from a condition called obstructive sleep apnea (OSA). This typically, but not always, affects those who snore. Men are affected more than women. Those who are overweight, with larger necks, and high blood pressure may be more vulnerable. OSA occurs when your throat muscles intermittently relax and obstruct breathing. This can be identified by the use of a portable continuous pulse oximeter that measures oxygen saturation while you sleep. Obstructive sleep apnea is diagnosed with repeated episodes of desaturation, where blood oxygen levels drop to <90%. In severe cases this can happen repeatedly throughout the night (greater than 30 per hour) with oxygen saturation <80%. There is another type of sleep apnea called central sleep apnea, where the same pattern occurs but is not caused by an airway obstruction, but rather when the brain doesn't send proper signals to the muscles that control breathing. Lastly, there's a final type of sleep apnea called mixed sleep apnea that occurs when both patterns occur throughout the night. Regardless of the type of apnea, this needs to be taken seriously and treated. Sleep apnea increases the risk of both heart disease and Alzheimer's. Those with sleep apnea often awake unrefreshed and are sleepy during the day.
Upper airway resistance syndrome (UARS) is another possible cause of airway obstruction. UARS is typically milder but has some overlapping features with sleep apnea and may progress to OSA if not treated. Sufferers are typically normal weight, often snore, are periodically awakened throughout the night, and excessively fatigued during the day. Because not everyone with sleep apnea or UARS has the typical symptoms or characteristics, we encourage EVERYONE to test their oxygen saturation throughout the night. This is not a definitive test for sleep apnea, but it can alert you to a potential problem.
You can ask your physician for a prescription to rent a continuous pulse oximeter or you can purchase a system to monitor your oxygen saturation at home. There are two products we like because of their medical grade accuracy. The first is the Innovo 50f Plus ($149.99) which is a snug fitting wristwatch that provides continuous monitoring of oxygen saturation and pulse rate with 24-hour data collection and analysis. You can use either Bluetooth or a cable to download the collected data to your personal computer (PC) via Windows. You can also easily use this device during the day to monitor your oxygen levels. The only downsides are that it isn't compatible with Apple or Android devices, and some people find it difficult to sleep with a tight-fitting watch. Another option is the BEDDR Sleep Tuner ($149) which is both Apple and Android compatible. BEDDR uses a small optical sensor that adheres to the middle of your forehead to measure blood oxygen levels and heart rate throughout the night. BEDDR provides a detailed report that you can see on your smartphone or tablet. The only downside to this device is that it's only practical for nighttime use.
If you find that you do have significant drops in oxygen saturation throughout the night, talk to your physician about setting up a formal sleep study. Many physicians are now arranging for home sleep studies. This is typically covered by insurance and will determine the treatment plan that may include a portable oxygen machine that provides Continuous Positive Airway Pressure, commonly called CPAP, to help treat this condition. Additional or alternate treatments may include a nighttime dental device or surgery. It's very helpful to monitor oxygen saturation levels throughout the night periodically once you've begun using a CPAP, to ensure that the treatment is effective.
Breathing
Anything that impedes your ability to breathe easily and deeply is likely reducing the flow of oxygen to your brain. If you feel pain or pressure when breathing deeply or find yourself feeling out of breath, make an appointment with your physician to determine the cause. Many conditions, including allergies, asthma, chronic obstructive pulmonary disease (COPD) such as chronic bronchitis or emphysema, and even cardiovascular disease can contribute to this impairment. Optimizing treatment is necessary to ensure maximum oxygen delivery to your brain.
Even those who are healthy often take incomplete or inadequate breaths from their chests (thoracic breathing), especially when they feel stressed or anxious. This can lead to an increased heart rate, dizziness, muscle tension, and more, as your blood isn't being properly oxygenated. Your goal is to switch to deep even breaths through your abdomen, called diaphragmatic breathing. To determine which type of breathing you're using, put one hand on your chest and one on your abdomen. Notice which area rises and falls with each breath. It's important to conduct this check especially when you're stressed.
Below is an exercise to encourage abdominal breathing for relaxation. You may perform this either standing, sitting or while lying down. Inhale slowly and deeply through your nose, keeping shoulders relaxed. Try to make your abdomen expand with each breath while your chest only rises very little. Exhale slowly through your mouth, keeping your jaw relaxed. You may hear a soft whooshing sound as you exhale. Repeat this exercise for several minutes. Observe how relaxed you feel afterwards. For those who aren't ready to jump into the expense of a nighttime or 24 hour continuous monitor, you may want to consider an inexpensive, small, portable, clip-on pulse oximeter that will allow you to spot check your oxygen saturation at any time. These inexpensive models do not collect data nor provide reports. We like the Innovo Deluxe ($27) which will easily allow you to monitor your oxygen saturation by clipping the device on the end of your finger, not unlike a clothespin, but much gentler. Pay attention to your readings when you're stressed and when you're relaxed. Your ultimate goal is to implement new ways of managing stress to facilitate full, deep breaths throughout the day. See
STRESS: Just Breathe
It's very important to breathe through your nose, as opposed to your mouth. This is true during the day, during exercise, and while we sleep. Nasal breathing produces nitric oxide, which improves your lungs' ability to absorb oxygen. Nitric oxide also increases the ability to transport oxygen throughout our bodies, including to our hearts and brains. Increased nitric oxide also helps our immune systems to fight off infections. Another advantage of nasal breathing is that our nose contains mucous membranes, cilia, and nose hairs that act as filters for pathogens and particulate pollutants. Most of us periodically have to breathe through our mouths when we're experiencing nasal obstruction, such as during a cold or when affected by allergies. If you find yourself mouth breathing when you're healthy, seek the help of a health or dental practitioner with expertise in this area. Chronic mouth breathing can lead to many detrimental health conditions including:
Dental complications, including gum disease, cavities, an unhealthy oral microbiome, and bad breath
Improper dental bite, problems with jaw joints
Higher incidence of snoring, sleep apnea, and poor sleep
Speech and swallowing issues
Enlarged tonsils and adenoids
Worsening asthma symptoms
Chronic health conditions including diabetes, heart disease, and even cognitive decline have been correlated with mouth breathing
Once you've ruled out or treated medical conditions that can lead to mouth breathing, try to retrain yourself to breathe through your nose. Be aware that stress can lead to mouth breathing. When we're taking shallow chest breaths, our blood is less oxygenated leading to mouth breathing. As you engage in ongoing stress management techniques, such as meditation, consciously focus on nose breathing to further maximize delivery of oxygen to your brain.
Circulation
A healthy cardiovascular system is continuously pumping and delivering oxygen to your brain and your body. Optimizing your cardiovascular health will optimize your brain health. One of the best and most effective ways to increase circulation throughout our bodies, but especially to our brains, is to exercise. We encourage you to set aside dedicated daily exercise time, while also increasing movement throughout the day. Those dealing with vascular issues may want to talk to your physician about trying Exercise With Oxygen Therapy (EWOT). To learn more and for ideas on how to use exercise to improve cognition, see EXERCISE: "Just Do It."
You'll find that as you apply multiple strategies in the protocol, your ABCs for oxygen delivery will continually improve. As you address any underlying insulin resistance, and adopt the KetoFLEX 12/3 lifestyle, your blood flow which carries oxygen throughout your body and to your brain, will continue to optimize. Over time, you may find that many other health parameters will also improve, underscoring the importance of monitoring any underlying chronic health conditions and working closely with your physician to reduce medication as needed.
© 2019 AHNP, LLC. All rights reserved. No part of this site or the content herein may be reproduced or reprinted without prior written permission from AHNP, LLC.
How can I lower my homocysteine?
02/06/20
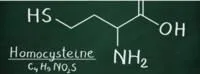
Optimal homocysteine is 7 micromolar or lower, and this may require the combination of three specific B vitamins, listed below, to achieve this goal:
- Vitamin B12 (as methylcobalamin, S-adenosylcobalamin, or hydroxocobalamin) at 1 mg per day. One commonly used combination is 0.5 mg of methylcobalamin plus 0.5 mg of S-adenosylcobalamin per day.
- Methyl-folate (folate is vitamin B9) at 0.8-5 mg per day. Start at the bottom end and only increase as needed.
- Pyridoxal-5-phosphate (P5P) at 20 mg per day (beware of high doses of pyridoxine over 150 mg, since these may cause nerve damage, making your feet feel numb and making it difficult to walk).
If high homocysteine persists, some add trimethylglycine (TMG) 500 mg (up to 3 g) once or twice per day. Additionally, those with the MTHFR (C667T) polymorphism may need to consider riboflavin (B2) supplementation. In this population, 1.6 mg of B2 reduces homocysteine by 40%. Also, be aware that adequate choline intake (550 mg for men & 425 mg for women) is necessary for homocysteine reduction.
ReCODE Trouble Shooting Checklist
If you are having trouble improving your cognition or reversing your symptoms, we have compiled a list to help you troubleshoot your program and get back on track.
- Are you checking ketones, and are you typically in the range of 1.5-4.0 mM BHB?
- Are you using exogenous ketones or MCT oil? Or able to achieve ketosis in the 1.5-4.0 range without?
- Is your score on BrainHQ or MoCA stable, declining, or improving?
- Did you rule out sleep apnea? Did your oximetry show no desaturation events at night?
- Did you heal your gut, then take probiotics and prebiotics (in food or as supplements)?
- Are you exercising at least 4x/wk? Doing both cardio and strength training?
- Do you have a health coach who can help keep things optimized? (Or a spouse or significant other who can do the same?)
- Do you have a practitioner who understands this approach?
- Are you using the Ketoflex 12/3 diet (or something similar)?
- Have you optimized hs-CRP (to <1.0), fasting insulin (to <5), hemoglobin A1c (to <5.6), vitamin D (50-80), hormones, and nutrients? Homocysteine <7? B12 >500? RBC Mg > 5.2?
- If these parameters are optimized, have you had a trial of WCFE (which increases BDNF)?
- Have you identified and treated all pathogens? If you have Borrelia, Babesia, Bartonella, or other pathogens, these should be treated—if possible, without using antibiotics (or, if antibiotics are used, monitor cognition carefully, and if there is a decline, move to a non-antibiotic approach).
- Have you identified and treated toxins (metallotoxins, organic toxins, and biotoxins)?
- If you have mycotoxins, have you been treated with cholestyramine (or other binding agents such as Welchol or clay or charcoal)? Had intranasal VIP? Cleared MARCoNS? Is your C4a back to normal? MMP9 back to normal?
- Is your glutathione level optimized?
BRAIN REHABILITATION

Save Your Brain and Reclaim Your Vitality
ENROLL In THIS 6 WEEK COURSE:
https://drknews.com/save-your-...
When the brain starts to degenerate, you often feel very, very tired. Brain-based fatigue is often overlooked, yet when combined with brain fog, depression, and memory loss, it is a serious red flag.
Sadly, both conventional and alternative healthcare professionals are not taught specifically how to diagnose or treat brain-based symptoms.
Here’s the interesting thing about brain health. You can’t use just anything to treat it; certain fundamental, foundational clinical steps have the biggest impact on changing the brain.
We go through each of these steps in each week of the program to teach you how to recognize your symptoms, change them, and then monitor your brain health. In this program you will:
- Stop treating symptoms.
-
Take a brain function assessment.
- Perform a self-neurological examination.
- Learn nutritional and lifestyle factors that can impact why you have declines in brain function.
- Learn exercises and other strategies to activate your brain.
- Learn dietary and nutritional steps to make a difference in how your brain functions.

https://online-learning.harvard.edu/course/cognitive-fitness?delta=0

